Book Travel Clinic Appointment
Altitude illness
What is it?
Altitude illness describes a number of problems that may occur when an individual ascends rapidly to high altitude, usually above 2,500m. As you gain altitude, air pressure decreases and so your body takes in less oxygen molecules per breath, leading to less oxygen being delivered around the body.
Risk areas
High altitude regions of the world such as the Himalayas (Asia), the Andes (South America), Rocky Mountains (North America), the Alps (Europe).
Popular high altitude destinations include Everest Base Camp and the Annapurna Circuit in Nepal (5,380m), Mount Kilimanjaro in Tanzania (5,895m), the Inca Trail in Peru (up to 4,200m), Aconcagua in Argentina (6,960m), Mount Kinabalu in Malayisan Borneo (4,095m) & Mount Fuji in Japan (3,776m).
Cities located at high altitude include: Lhasa, Tibet (3,658m); La Paz, Bolivia (3,630m); Cuzco, Peru (3,399m); Quito, Ecuador (2,819m); Bogotá, Colombia (2,644m); Addis Ababa (2,408m) and Johannesburg, South Africa (1,750m).
Prevention (holistic)
The best way to prevent altitude illness is by acclimitasing slowly and allowing for rest. It is also important to be aware of symptoms of altitude illness and always attempt to descent if these symptoms worsen at a given altitude or if they are severe.
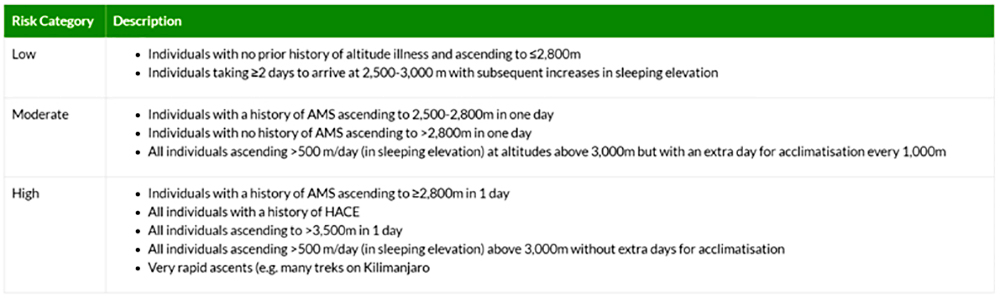
Table 1: Wilderness Medicine Society Risk categories for Acute Mountain Sickness
Prevention (medication)
Medication is not necessary for low risk, with gradual ascent sufficient for individuals. For moderate or high risk ascents, preventative medicine may be considered in conjunction with gradual ascent. Acetazolamide (Diamox) is the preferred medicine but is unlicensed for this indication.
Please discuss your requirements with our Travel Pharmacist or Nurse.
Further information
For more information, please visit the following link:
https://travelhealthpro.org.uk/disease/12/altitude-illness
Cholera
What is it?
Cholera is bacterial infection that is characterised by watery diarrhoea. It is commonly caused by contaminated food and water.
Signs and Symptoms
The initial symptoms of Cholera can begin anywhere between 1-5 days after ingesting the bacteria. Sufferers can experience vomiting of a clear liquid, and painless diarrhoea, which is pale and cloudy in appearance. These symptoms can expel a massive amount of fluid from the body, resulting in dehydration and causing the skin to turn a greyish blue colour.
Risk areas
Common in many low-income countries and is associated with poor sanitation and poor access to clean water. The overall risk for travellers is very low but the risk is far greater for those living in unsanitary conditions, for example relief workers in disaster or refugee areas.

The disease is endemic in Africa, Asia, Central and South America and is prevalent in areas where there is poor sanitation.
Prevention
Following good personal hygiene and safe food and water practices can help reduce the risk of acquiring cholera.
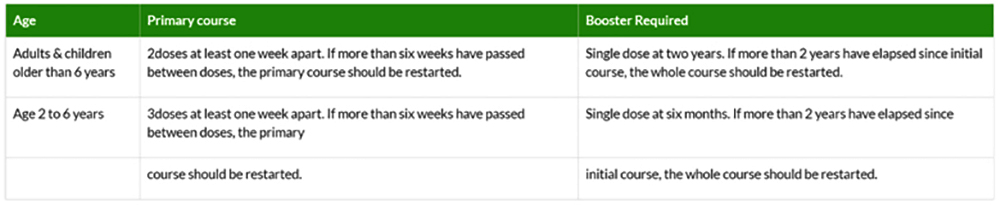
Vaccine schedule
Dukoral, a licensed vaccine effective against cholera, is available in the UK. It is not recommended for most travellers but for those whose activities or medical history puts them at increased risk. This includes:
- Aid workers
- Those going to areas of cholera outbreak and who will have limited access to safe water
Hepatitis A
What is it?
Hepatitis A is a highly infectious virus that can cause inflammation of the liver. The virus is most commonly transmitted through food or water that has been contaminated by human faeces or by direct contact with an infected person.
Signs and Symptoms
It can take up to two weeks for any signs or symptoms develop and the severity of the virus ranges; in young children, infection may show mild or no symptoms, but it can be a serious illness in older people. Common signs and symptoms of Hepatitis A include: fever, muscular aches, nausea, vomiting, diarrhoea, weight loss, abdominal pain and yellow discolouration of the skin and eyes.
Risk areas
Hepatits A occurs worldwide, but areas with high levels of infection include low-income countries where there is poor sanitation or hygeiene practices. High risk areas include:
- The Indian subcontinent
- Subsaharan and North Africa
- Parts of South East Asia
- South & Central America
- The Middle East
Prevention
The most common route of infection in travellers is consumption of contaminated food or water. Simple measures to reduce the risk of infection include
- drinking water from a sealed source or boiled water,
- avoiding ice made from unpurified water,
- avoiding salad that may be washed with tap water and
- ensuring food has been freshly cooked and is hot
Vaccine schedule
There are several effective Hepatitis A vaccines available for travellers who intend to visit areas where Hepatitis A is common. Some of these vaccines have been combined with Typhoid and Hepatitis B.

Length of protection
The duration of protection from a completed course of Hepatitis A vaccine is a minimum of 25 years.
Hepatitis B
What is it?
Hepatitis B is a viral infection that affects the liver. It is spread by direct contact with the blood or bodily fluids of an infected person.
Signs and Symptoms
The signs and symptoms of Hepatitis B include mild fever, flu-like symptoms, high temperature, gastro-intestinal upset, nausea and vomiting, diarrhoea and abdominal pain, yellow skin and eyes.
Risk areas
Hepatitis B occurs worldwide but it’s distribution is higher in some areas of the world such as:
- East Asia
- Sub Saharan Africa
- Amazon basin
- Southern parts of Eastern & Central Europe
- Middle East
- Indian Subcontinent
The general risk to travellers is low, although certain behaviours or activities increase the risk, especially in areas where Hepatitis B infection is more common. Risk factors include:
- Unprotected sex
- Exposure to blood i.e. via healthcare
- Exposure to contaminated needles through injecting drug use or dental work
- Contact sports
- Adoption of children from risk countries
- Long stay travel
Prevention
Avoiding contact with blood and body fluids can help reduce the risk of transmission. Unprotected sexual intercourse should be avoided, as should tattoos, piercings and other contact to needles (unless sterile). If travelling to remote or poor areas, it may be prudent to carry a sterile medical equipment kit in case of accidents.
Vaccine schedule
There are several well-tolerated hepatitis B vaccines, including combined hepatitis A/B products, and vaccination is recommended for all travellers considered at risk.
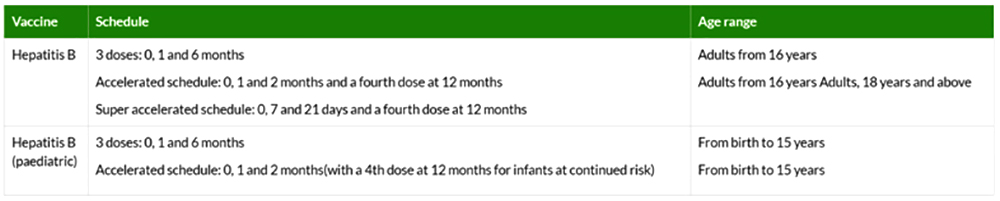
Length of protection
For individuals at continued risk, a single booster dose should be offered, once only, 5 years after primary immunization has been completed. For most travellers that have completed their primary course, a booster at 5 years is usually unnecessary. However, any risk factors that increase risk should be discussed with your Travel Clinic Pharmacist or Nurse.
Japanese Encephalitis
What is it?
Japanese Encephalitis is a mosquito borne illness that can cause inflammation of the brain, and is potentially fatal. It is spread through infected mosquitos mainly from sunset to sunrise.
Signs and Symptoms
Symptoms usually occur 5 to 15 days after being bitten by an infected mosquito. Initially, a flu-like illness may occur, which may progress to brain swelling, resulting in symptoms such as high fever, confusion, convulsions, headache, neck stiffness and paralysis. Japanese Encephalitis can result in death or permanent brain damage and disability.
Risk areas
Despite the name, Japanese Encephalitis is endemic in 24 countries across Asia and the Western Pacific, not just in Japan. It is most common in rural areas where there is rice growing and pig farming, although it can occur in urban areas too.

The risk to travellers is generally very low, however it can increase significantly for persons who intend to live or travel in risk areas for long periods of time or who visit rural areas during transmission seasons. It should be noted that even short trips (fieldwork, camping or night time exposure) can significantly increase the risk to travellers.
Prevention
Bite avoidance, especially between dusk and dawn, can help reduce the risk of getting Japanese Encephalitis.
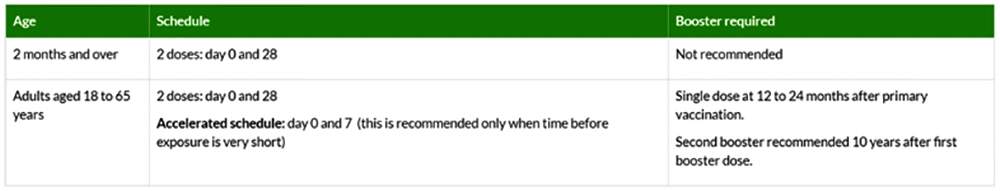
Vaccine schedule
There is a licensed Japanese Encephalitis vaccine that is recommended forindividuals who plan to stay in rural areas where Japanese Encephalitis occurs during the main transmission season or those whose activities put them at greater risk.
Meningococcal Meningitis ACWY (Menveo)
What is it?
Meningococcal disease is a uncommon but potentially life-threatening infection caused by different strains for a bacteria species (Men A, B, C, W, Y and X).
Around 10% of the UK population carry the meningitis bacteria in their nose and throat. It is spread between individuals by kissing, sneezing, coughing or during close contact with a carrier. Carriers of the bacteria generally don’t have any symptoms but can develop the disease in certain cases.
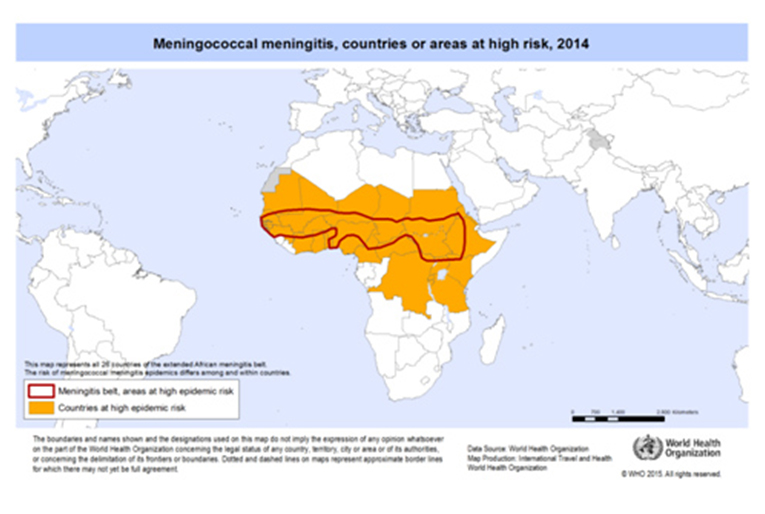
Risk areas
The disease is most common in the ‘meningitis belt’ of sub-Saharan Africa, stretching from Senegal through to Ethiopia. Following several large outbreaks of the disease in Saudi Arabia, certification of vaccination (with the quadrivalent vaccine) against Meningitis ACWY is now mandatory for pilgrims.
Prevention
Travellers to areas within the meningitis belt are at increased risk for a number of reasons such as:
- Long term stay with close contact with local population
- Healthcare workers
- Those visiting friends or relatives
- Backpackers
Vaccine schedule
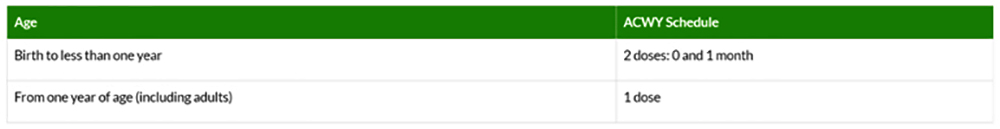
Length of protection
Booster dose can be considered after 5 years following primary vaccination.
Hajj & Umrah
We have plenty of experience vaccinating pilgrims travelling to perform Hajj and Umrah and our clinics are among those recommended by the Muslim Council of Britain (MCB). We can vaccinate you for Meningitis ACWY and give you the certificate required by Saudi Arabia for the visa. We can also offer other vaccines such as hepatitis A, hepatitis B and seasonal flu (at certain times of year) that are recommended by the Saudi Ministry of Health. Many of our staff have performed Hajj and are well placed to discuss questions you may have about your pilgrimage.
Rabies
What is it?
Rabies is a viral disease that is spread by a bite or scratch from an infected animal, usually a dog. It affects the brain and spinal cord and once symptoms are present, it is nearly always fatal. Rabies is estimated to caused around 60,000 human deaths worldwide each year.
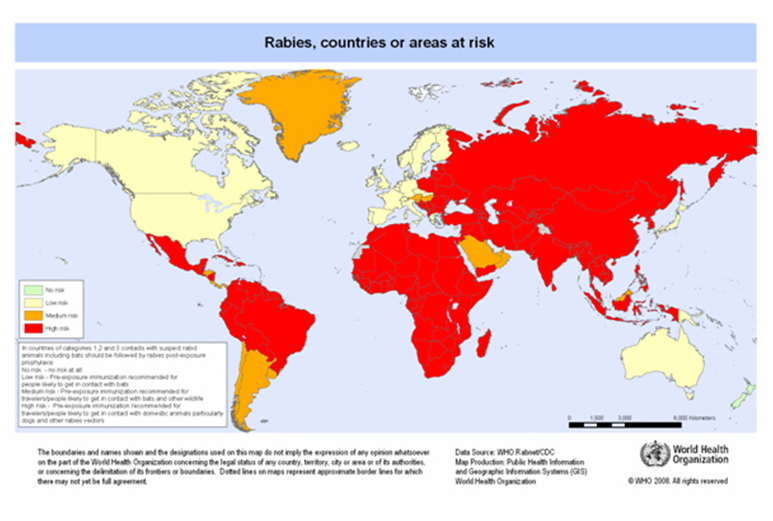
Risk areas
Rabies is endemic throughout most of the world.
Prevention
Contact with wild or domestic animals should be avoided by travellers. The following steps should also be taken following potential rabies exposure:
- Immediately wash wound with soap & running water for several minutes
- Apply a disinfectant to the wound such as iodine or 40-70% alcohol
- Apply a simple dressing to the wound
- Seek medical advice as soon as possible
Vaccine schedule
Rabies vaccine is recommended for pre-exposure protection to travellers whose activities put them at increased risk. This includes:
- Those visiting areas where access to post-exposure treatment is limited
- Those planning high risk activities such as running or cycling
- Long-stay travellers (more than one month)
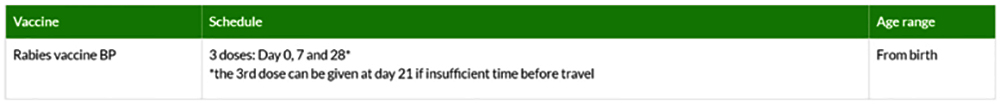
Length of protection
- Infrequent risk – booster dose to be considered at 10 years post primary course
- Frequent risk – booster at 1 year and then booster every 3 to 5 years
- *Berkeley Court Pharmacy Travel Clinic provide the intramuscular Rabies injection. Please note that we do not currently provide the intradermal vaccine as this method is not currently licensed for use in the UK. For further information please visit the link below:
http://wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/perspectives-intradermal-rabies-preexposure-immunization - Further information provided by the Green Book can also be found by visiting:
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/85762/Green-Book-Chapter-27-v3_0.pdf
Tetanus, Diptheria& Polio
What is it?
The combined injection protects against three different diseases. Tetanus is a vaccine-preventable disease that is caused by toxins produced by bacteria found in soil worldwide. Polio is a potentially paralyzing, vaccine preventable viral infection that is transmitted through food or water contaminated by human faeces or direct contact with an infected person. Diptheria is a bacterial infection that is spread by exhaled water droplets, especially when in close contact with local population of endemic countries.
Signs and Symptoms
Tetanus symptoms take time to develop, with the incubation period lasting between 4 and 21 days. The earliest symptom is lockjaw, a severe stiffness in the mandibular muscles which makes it very difficult to open your mouth. This stiffness, which is often accompanied by spasms, spreads to the neck and limbs over the following period of up to three days. It can become difficult to swallow, with severe cases causing difficulty in breathing, which can lead to suffocation.
Polio is highly infectious, but symptoms do not typically appear for up to 20 days. Early symptoms include fever, headaches, vomiting, fatigue, chest pains, and stiffness in the neck. In rare cases (1 in 200), the sufferer can be permanently paralysed, usually in the legs. Among these rare cases, 5-10% can be killed when their breathing muscles become immobilised.
Other symptoms include a high fever, high blood pressure, rapid heartbeat and heavy sweating.
There is no cure for Polio; it can only be prevented against. In the UK, the TDP vaccination is part of the childhood immunisation schedule - this injection prevents
against Tetanus, Diphtheria and Polio. Travellers to areas at risk may be recommended a single injection of Revaxis.
Prevention
Travellers to areas at risk may be recommended a single injection of Revaxis, which also covers against Diphtheria and Polio. In the UK, the TDP vaccination against Tetanus infection is part of the childhood immunisation schedule.
Risk areas
Tetanus is found worldwide but is generally more common in countries with poor vaccination coverage. Polio is now only endemic in Afghanistan and Pakistan but it can be imported to other countries by infected individuals. Diptheria can be found worldwide but is more common in developing countries where vaccination coverage is not as widespread.
Vaccine schedule
Travellers should have completed or be up-to-date with a primary vaccination course according to the NHS vaccination schedule.
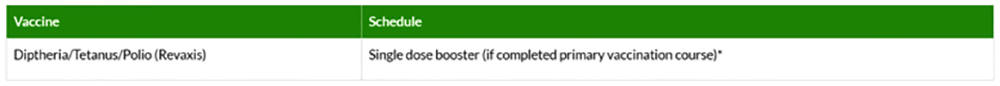
*The primary course of diphtheria, tetanus and polio (DTP) is part of the standard UK childhood immunisation programme. If you have received the primary course, you may need a booster of one dose. If you have not received a primary course previously, you may require a course of three vaccinations.
Length of protection
10 years
Tick-borne encephalitis
What is it?
Tick-borne encephalitis is a viral infection spread through the bite of an infected tick. It can also be spread via unpasteurized milk from infected cows, sheep and goats.
Signs and Symptoms
The initial symptoms of Tick-borne Encephalitis usually occur one to two weeks after a tick bite and include fever, headache and general flu-like illness. Sufferers may also complain of nausea, muscle pain, lethargy and general discomfort. Some patients may go on to develop Encephalitis, which can cause paralysis and can be fatal in some cases.
Risk areas
The disease occurs in parts of central, northern and Eastern Europe, Siberia and parts of Asia. In Europe, early spring through to late autumn are generally higher risk, however seasons vary by location. Travellers to areas where Tick-Borne Encephalitis is present may be at risk when walking, camping or working in woodland areas.
Prevention
Travellers should avoid known heavily tick-infested areas of forest and woodland during transmission seasons. Bite avoidance measures should also be employed when in risk areas and body should be checked regularly for ticks.
Insect bite avoidance methods should be taken, such as wearing protective clothing and using insect repelle
City of Westminster
Greater London
NW1 6AE